Professor Rao’s Research
“I am honoured to receive the Daniela Dwyer Foundation Fellowship. This support has allowed the Rao Laboratory to accelerate progress of our non-invasive liquid biopsy tests of blood samples to monitor in real-time, cancer progression and provide novel combinations of drugs for patients via personalised medicine approaches. We are very close to getting accreditation for clinical testing so the testing can be utilised by labs around Australia and worldwide.
We are very grateful for the support of the Daniela Dwyer Foundation.”
– Sudha Rao
Professor Rao and her team are making rapid advancements in the following important novel areas:
Digital Pathology Diagnostic Platform: Early intervention blood tests to detect brain cancer or brain metastasis
Professor Rao’s Lab has established the world-first liquid biopsy digital pathology platform – a blood test that combines expertise in epigenetics, digital pathology and measuring and characterising cancer cells in the blood. For the first time, they have been able to monitor the ‘“seeders of metastasis”’ (metastatic initiating cells) – the cells that spread cancer. These ‘seeders’ are critical initiators of metastatic brain cancer and may play a role in primary brain cancers such as glioblastomas. Monitoring these ‘seeders’ has not previously been possible. But now, the Rao Lab has identified the precise molecular/protein make-up of these metastatic initiating cells (MITS) and is now working on validating and characterising the molecular and protein make-up of the metastatic cells that are brain specific metastatic initiating cells (bMITS).
Using novel technology platforms (not available elsewhere in Australia) and a novel digital pathology platform, the Rao Lab has developed a blood test to identify these bMITS that allows monitoring of these ‘seeders’ before they metastasise to the brain. This also has the potential to diagnose brain metastasis or recurrence of primary brain cancer early. This will enable treatment to intervene when the patient has the highest chance of a successful outcome.

Clinical Diagnostics for brain cancer patients – Personalised medicine
It is essential that therapeutics for brain cancers and brain metastasis act rapidly given the quick progress of these cancers, to target the cancer cells causing primary or metastatic brain cancers and to re-invigorate and allow the patient’s own immune system to kill the cancers. The Rao Lab has pioneered methods using novel technologies that allow in-vitro screening of a patient’s specific live cancer cells to determine which drugs the cancer may respond to.
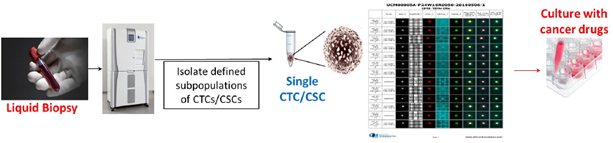
This method addresses the key dilemma oncologists face in not knowing what drugs (such as chemotherapy, or immunotherapy) will be effective for the patient, who is already very sick. A test showing if a patient is likely to respond to a specific treatment reduces the time the oncologist may need to find an effective treatment. Early intervention means a higher chance of a positive outcome. Oncologists could provide individual assessments of the correct treatment, and prioritise patients who may respond to specific therapies.
The Rao Lab has identified an epigenetic marker that is a central switch in resistance to many types of therapeutics. Using this marker, the Lab’s novel blood test predicts and tracks, in a non-invasive manner, the patient’s responsiveness to therapeutics. The Rao Lab has successfully used this technology with a small group of patients to guide the use of immunotherapy for Melanoma.
The Rao Lab will also refine and validate the novel signature for brain metastatic targeted CTCs and primary brain cancer CTCs. This will enable us to further understand the features of CTCs that come from primary brain cancers or migrate to brain metastases.
Further funding will help establish this blood test as routine, giving many cancer patients personalised medicine options to prolong survival.
Summary
Professor Rao and her researchers work closely with a team of committed neurologists and oncologists. The Rao Lab’s early intervention approaches are being taken seriously as a matter of urgency. Currently, primary brain cancer patients deal with invasive surgery, chemotherapy and radiotherapy with a high rate of recurrence. Unfortunately, surgery is not always possible and there are minimal to no treatment options available. The Rao lab has made game-changing developments for early intervention by tracking cancer in the blood before it reappears. As a result, these developments provide an important opportunity for the development of targeted drugs that can destroy these aggressive cancer cells before they metastasize. This screening allows for a personalised approach.
With funding, the Rao Lab will work closely with oncologists to accelerate the progress of these blood tests and drug screening platforms. This will enable them to become a routine part of clinical practice for brain cancer patients. Through this early intervention, the patient can be treated with close, non-invasive monitoring before the cancer returns. Additional funds will refine this signature, develop diagnostic tests and therapeutic targeting to allow this work to move from the bench to the clinic.
The Rao Lab currently has blanket ethics for patient recruitment at the Canberra Hospital, Royal Brisbane Women’s Hospital (RBWH) and Monash University Hospital, and is working closely with oncologists to identify and recruit patients with a focus on primary and metastatic brain cancers.